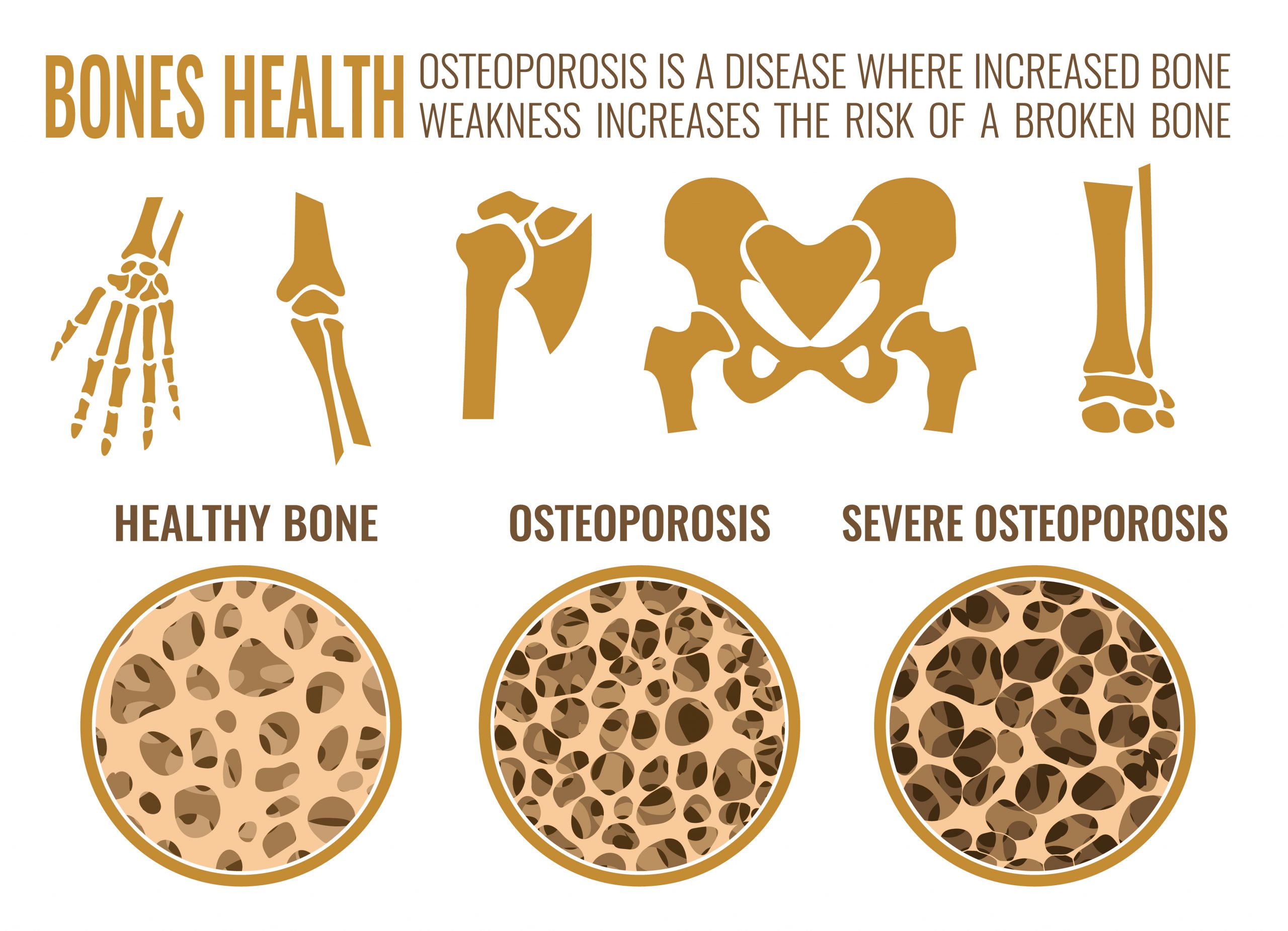
Osteoporosis is a ‘silent’ condition which increases the risk of serious fractures and it is most commonly due to a loss of bone density. Fractures occur most commonly in the wrists, hips and spine and are often due to minimal trauma (eg tripping, falling out of bed or a chair). Some older adults may appear or comment that they have become shorter with age or have a ‘hump’ on their back. This is mostly due to vertebral fractures in their spine, leading to a loss of height.
Fractures are associated with pain, decreased mobility, loss of function and an overall decreased quality of life.
In a recent report from the Australian Institute of Health and Welfare (AIHW, a branch of the Australian government) it is estimated that approximately 924,000 Australians (about 3.8% of the population) have osteoporosis. Its prevalence is most common in older women, occurring in about 1 in 4 women aged over 75.
Additionally, there were around 92,321 hospitalisations in 2017-2018 for fractures in patients aged 50 and over. Unfortunately, the risk of having a second fracture is about 50%, and about 4 times more likely to occur within the next year.
Women are more likely to develop osteoporosis, especially after menopause (due to the reduction in oestrogen which is protective for bone health). Men do get osteoporosis as well but generally not until later in life, due to the gradual decline in testosterone with age.
What puts me at risk of developing osteoporosis?
Besides age and female gender you may be at risk if:
- there is a family history of osteoporosis (especially in first degree relatives – eg mother)
- a reduced calcium intake
- low vitamin D levels
- certain medical conditions will put you at risk as well. These include:
- taking steroid medication for long periods of time (tablets not inhalers though)
- malabsorption: eg coeliac disease, inflammatory bowel disease
- thyroid conditions
- other chronic diseases, such as rheumatoid arthritis, chronic kidney disease
- medications such as those for treatment of epilepsy, breast cancer, prostate cancer and depression
- being a smoker
- excessive alcohol intake
- weight: either being thin or overweight
How will I know whether I have osteoporosis?
As osteoporosis is generally a ‘silent disease’ (ie. most people will not be aware of it until they have a fracture) it is a good idea to see your general practitioner to see if you may be at risk and if further investigations are required. Your doctor will go through your medical history, as well as family and lifestyle history to see if you are at risk.

Tests to diagnose Osteoporosis
Your doctor may refer you to have bone densitometry test (BMD or DXA scan). There are Medicare rebates available if you have had a previous fracture due to minimal trauma OR are over the age of 70 years.
This a painless test which looks at your bone density in the spine and hip (two common areas where fractures may occur). There is some radiation involved but it is relatively low compared to other x-rays (about 10% of the radiation of an x-ray).
You will receive 2 scores:
T-score – comparing your bone density to the bone density of younger adults
Z-score – comparing your bone density to the bone density of those of a similar age
A diagnosis of osteoporosis is made using the T-Score:
- A score of 1 to -1 is a normal result
- A score of -1.0 to -2.5 indicates osteopenia (meaning you may be at risk of developing osteoporosis)
- A score of -2.5 or less means that you have osteoporosis
It is important to note that this test will not diagnose if you have had a vertebral fracture (unless it happens to be in the area being scanned). Vertebral fractures are usually diagnosed on x-ray or may be picked up incidentally, such as on a chest x-ray.
What can I do to reduce my risk of developing osteoporosis?
Unfortunately, if you have a family history or any of the medical conditions described above, you will be at higher risk. But there are a number of other strategies you can take to reduce your risk. These include:
- Maintaining an adequate calcium intake, especially as you get older. This may need to be increased with increased age due to increased loss of bone, decreased gut absorption as well as loss though the kidneys. Osteoporosis Australia recommends 3-5 serves of calcium daily. Most people require 3 serves of dairy per day to obtain enough calcium. 1 serve of calcium = 250 mL milk, 200 g yoghurt or 40 g cheddar cheese.
If you are not able to get enough calcium through diet alone you can take a calcium supplement. A dose of 1000 to 1300mg a day is recommended. The most common supplements available are calcium carbonate and calcium citrate. These can be purchased over the counter at most pharmacies or supermarkets. - Having adequate vitamin D levels – vitamin D helps to increase the absorption of calcium. The easiest way to get this is from exposure to sunlight, usually a few minutes a day. Vitamin D levels tend to be lower in winter, in the elderly, those with darker skin and those who cover up due to religious reasons. Supplementation is available and dosages varies from around 800 to 1000IU a day in those with vitamin D deficiency (which can be diagnosed on a blood test).
- Stopping smoking and decreasing your alcohol intake. As well as other health benefits, this will help to reduce your risk of developing osteoporosis.
- Maintaining a healthy weight. Keeping your BMI (body mass index) in a healthy range based on your weight and height. See here to calculate your BMI http://healthyweight.health.gov.au/wps/portal/Home/helping-hand/bmi
A BMI of 20 to 25 is recommended. - Take regular exercise, helping to improve and maintain bone density as well as improve strength and reduce your risk of falls. Recommended exercises include: weight bearing exercise (such as walking), resistance training (eg lifting light weights, pulling on elastic straps). It is recommended to exercise for at least 30min at least 3 times a week.
Preventing fractures and falls
Avoiding fractures is the main concern for those with osteoporosis. Once you have had one fracture, a second or third is more likely. Many fractures are caused by falls – people aged 65 years and older are most likely to be affected. Falls can cause serious injuries and damage self-confidence and independence. Preventing falls is an important way to reduce your chance of fractures. Your doctor, physiotherapist or occupational therapist can advise on ways to reduce your risk of falling, including:
- exercises to improve muscle strength
- ‘fall-proofing’ your house (eg securing loose floor rugs and electrical or phone cords, using a non-slip mat for the bath or shower, fixing poor lighting)
- checking your vision
- ensuring the medicines you take are not affecting your balance
- checking your strength and whether a walking aid would help you.
Prescribed medication
If you have had a fracture due to osteoporosis or have been diagnosed with osteoporosis and are at high risk of fractures your doctor may recommend medication for you.
These include:
Bisphosphonates:
Such as alendronate (Fosamax), risedronate (Actonel), zoledronic acid (Aclasta – which is an intravenous infusion). These medications are subsidised by the Pharmaceutical Benefits Scheme (PBS) for those who have been diagnosed with a fracture and osteoporosis OR those over the age of 70 with osteoporosis (and no previous fracture). Patients who are also on long term steroid medication (check with your doctor) may also be eligible under the PBS.
These medications can increase bone density by up to 50 to 70%. They come either tablet form (daily, weekly or monthly) or intravenous infusion once a year (usually done at your GP practice).
Denosumab (Prolia)
This medication is given by injection (under the skin – ‘subcutaneously’) every 6 months. It can be given at your usual GP practice. It works differently to the bisphosphonates but can reduce spinal fractures by up to two thirds. It is available on the PBS for the same indications as listed above.
Selective Oestrogen Receptor Modulators (SERMs) – raloxifene (Evista)
This medication is used in post-menopausal women for the treatment and prevention of osteoporosis. It is currently on the PBS for these women who have osteoporosis with a previous fracture. As well as reducing the risk of fractures, raloxifene reduces the risk of invasive breast cancer in women with a personal or family history of breast cancer.
Teripatide (Forteo)
This medication is self-administered by daily injection and is PBS listed for those with severe osteoporosis for 18 months. It is restricted to patients who have previously been on other medications for their osteoporosis and must be prescribed by a specialist.
Hormone Replacement Therapy (HRT) in post-menopausal women
This medication is usually indicated for women with menopausal symptoms and low bone density below the age of 60. Once over the age of 60, the risk may outweigh the benefits (with increased risk of heart disease, stroke, and breast cancer). Most doctors recommend considering alternative treatment options once you reach the age of 60 years.
For further information please see: