Are you suffering from knee pain due to your osteoarthritis? We are currently looking for participants to trial a new intraarticular (into the joint) injection to assess its ability to provide both rapid and sustained relief from osteoarthritis pain and delay need for future joint replacement surgery.,
What is osteoarthritis?
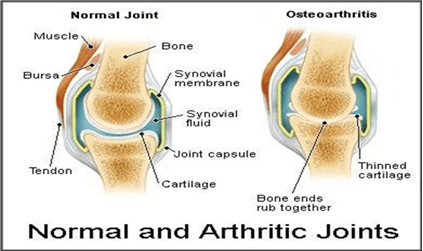
Osteoarthritis (OA) is a degenerative condition of the joints mostly affecting the hips, knees and ankles.
Symptoms people may experience include pain, joint stiffness, and decreased joint movement which may get progressively worse over time.
In osteoarthritis the cartilage which cushions the joint wears away. This can lead to the bones in the joints rubbing together causing inflammation and changes in the surrounding bones. The incidence of OA is increasing due to an increase in our ageing population, as well as the increased prevalence of overweight and obesity in modern society.
Source: Guideline for the non-surgical management of hip & knee OA, RACGP 2009
Who gets osteoarthritis?
Osteoarthritis is more common in adults over the age of 45 (and especially in those over 65 years). It affects up to 8% of Australians and is more prevalent in females than males.
What are the risk factors for osteoarthritis?
- being female
- joint misalignment (especially if you have had abnormalities from birth)
- a history of joint trauma or injury
- being overweight-
- doing activities which place excessive load on your joints (ie. Doing jobs that require frequent heavy lifting)
- if you have a family history of osteoarthritis.
How can I prevent the likelihood of getting osteoarthritis?
You can do this my maintaining a healthy diet, achieving a healthy weight, stopping smoking and maintaining a moderate level of physical activity.
Management of Osteoarthritis
A good place to start is by seeing your general practitioner. Your GP can help to diagnose, discuss various management strategies, and referral to other health professionals if needed.
What treatment options are there for osteoarthritis?
1.Education and self- management
Gaining an understanding about the nature of your condition and what you can do to manage your symptoms can help you to feel less anxious and more empowered about the management of your OA.
Sources of information regarding OA can be obtained from your GP, other health professionals, or calling the Arthritis Helpline on 1800 011 041.
You can also find more resources from Arthritis Australia at https://arthritisaustralia.com.au/get-support/resources/
These include self- help workshops, online videos and links to other resources.
2. Medication
Paracetamol is one of the first line treatments that are used to help reduce pain. These can be taken either on a as needed basis (ie. when you experience the pain) or regularly (to provide more to consistent around the clock pain relief). Paracetamol is available over the counter (no prescription required) but always check with you pharmacist or GP to make sure it does not interact with other medication that you may be taking)
The next line treatments are NSAIDs (non steroidal anti-inflammatory drugs). These are intended to reduce pain by reducing inflammation. There is a group of NSAIDs that are prescribed specifically for arthritis pain but with less side effects on the stomach and intestinal system. These are known as COX-2 inhibitors. These are available on prescription only so you will need to discuss whether these are suitable for you with your doctor. Unfortunately, they are only intended to be used for short term use only rather than long term. Care needs to be taken in people with a history of heart disease, high blood pressure , smoke or have diabetes due to the increased risk of stroke and heart attack with this medication long term.
Corticosteroid injections into the joint (intra-articular) can also provide short term relief of pain and inflammation. These can provide relief anywhere from 4 weeks to 3 months in most people and can be repeated up to four times a year.
Another type of injection that can be used in the joint is hyaluronic acid injections. This can be used in those with mild to moderate pain, swelling and stiffness. Benefits can take a slightly longer to be noticed than corticosteroid injections but can last longer, up to six months. Patients may only require 1 to 2 injections to get noticeable benefit, but this therapy can be more costly.
As a last resort, oral opioid analgesics may be needed to relieve severe pain.
3. Exercise and physical therapy
This can help to strengthen muscles around the joints and improve joint stability and flexibility.
This should be done under the supervision of a qualified professional such as a physiotherapist or exercise physiologist. Your doctor may be able to suggest suitable programs to assist with the above.
Examples of suitable exercises include – cycling, walking, swimming.
Mechanical aids such as walking sticks, orthotics can also be useful in helping to reduce the pain and improve function.
4. Weight loss and diet
Another way to reduce the stress on your joints is by losing weight if you are overweight or obese.
Those with obesity have a 20 times increased risk of developing bilateral OA of the knee. For every 2 units of BMI gain (equal to about 5kg), the risk of OA in the knee increases by approximately 36%. Conversely, for every 5kg decrease in body weight during the preceding 10 years, the risk of knee OA declines by more than 50%.
Most people can expect an up to 30% improvement in joint pain and function after just losing 5% of their body weight.
Ways to reduce intake:
- reducing your intake of saturate fats
- reducing your sugar intake
- eating plenty of fruits, vegetable and wholegrain foods
- reducing your alcohol intake.
A dietician can help provide guidance with your diet.
5. Other therapies
This can include topical medications such as topical NSAIDs in the form of gels and creams. Another medication can be helpful such as Capsaicin gel. These can usually be used in conjunction with oral pain medications that you may already be taking.
6.Surgery
Joint replacement is usually recommended in severe cases of osteoarthritis, in particular in those with severe pain impacting on their mobility and quality of life. Knee replacements can last on average 10 – 12 years. Exercise and losing weight prior and after your surgery can greatly improve your recovery from surgery and if well cared for (ie. by maintaining a normal weight) increasing the lifespan of your knee replacement.

